Important Note: This Help Center Article is no longer relevant for the current calendar year. This Help Center Article is retained in the event of an audit for fidelity of information to align with changes over time and so we keep this article hosted. If you are looking for current calendar year information please ensure the calendar year is included in the title of the Help Center Article.
Contents
The Quality Payment Program (QPP) is a federally mandated Medicare program by Centers for Medicare and Medicaid Services (CMS) that seeks to improve patient care and outcomes while managing the costs of services patients receive.
Clinicians may participate in the Quality Payment Program through one of two tracks:

The Merit-based Incentive Payment System (MIPS) is the primary way to participate in the Quality Payment Program. Advanced Alternative Payment Models (APMs) are optional programs that offer different incentive structures for high quality, cost efficient care.
MIPS is the standard fee-for-service (FFS) payment track that applies to around 95% of physicians (before the pandemic exception opportunities). Under MIPS, CMS evaluates performance across four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. Here is a brief description of each category from CMS:

The following Clinician Types are eligible for MIPS:
- Physicians (MD, DO, DDS, DMD, DPM, OD)
- Osteopathic practitioners
- Chiropractors
- Physician assistants
- Nurse practitioners
- Certified nurse anesthetists
- Physical therapists
- Occupational therapists
- Clinical psychologists
- Qualified speech-language pathologists
- Qualified audiologists
- Registered dietitians or nutrition professionals
- Clinical social workers
- Certified nurse-midwives
- Clinical nurse specialists- new in 2023
If any of the following apply to the provider, they are not required to participate in MIPS:
- Fewer than 200 Medicare fee-for-service patients
- Less than $90,000 in Medicare charges
- Fewer than 200 Medicare fee schedule services
- Participate in an Advanced APM
- First-year Medicare provider
Use the CMS’s Participation Lookup website to confirm eligibility.
Interpreting Eligibility
Once practices find the “Associated Practice” that is using Elation, there are three possible outcomes, only one of which requires practices to participate in MIPS.

Eligibility note: if you or your practice are associated with and participating in an APM (ACO or other APM type) contact the APM administrator to determine best practices for MIPS participation and data submission. MIPS APM participation may vary from traditional MIPS participation.
Each of the four performance evaluation categories has different requirements that need to be met and each practice’s goal is to maximize points earned. This year, CMS has weighted the categories as follows:
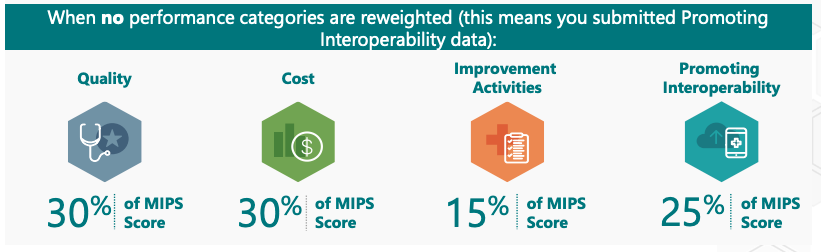

One of the highest weighted categories is Quality, which looks at Clinical Quality Measures.
Practices can submit as many measures as they want but are scored on their 6 top-performing quality measures. Data needs to be collected for these measures across at least 70% of their visits. Elation has 10 quality measures that we can report on and with a set of videos that cover workflows. You can also learn more about all the Clinical Quality Measures that Elation supports in the Clinical Quality Measures Reports Guide.
- Important Note: One (1) of the 6 measures must be an outcome measure. The outcome measures available in Elation are:
- Controlling High Blood Pressure
- Diabetes HbA1c: Poor Control
Each measure is scored out of 10 points. Their score depends on how many patients are meeting the requirements of the measure. For each measure, a practice earns a percentage first, which is then converted to a score out of10 based on benchmarks. The average score for each 6 measures determines how many points they earn out of 30. Their performance is also compared to their peers and against annual benchmarks to determine the absolute number out of 10. The better they perform against their peers, the higher their score per measure will be.
Practices who have 15 or fewer providers under a Tax ID Number will automatically earn 6 extra points towards their Quality numerator.
Cost is captured via the codes that are submitted via claims and measure Medicare spending per beneficiary and total per capita cost. Practices don’t need to complete any specific actions in Elation or submit anything for this category. To optimize your scoring potential in this category, we recommend taking steps as a practice to minimize overall cost and hospitalizations for your patients.
For this category, CMS publishes a list of activities that are intended to improve care and outcomes. This is typically an easy category for practices to earn points. You can also learn more about Improvement Activities in our Improvement Activities (MIPS 2023) guide.
Most practices need to pick and complete 2-4 improvement activities to receive the maximum score of 40 points in this category. Improvement activities are classified as either medium-weight (10 points) or high-weighted (20 points), and the number and type of activities to maximize points depends on a practice’s size.
This category requires 4 objectives, 2 registry integrations, a security audit and a few attestations. Learn more about the Promoting Interoperability Performance Category in the Promoting Interoperability (MIPS 2023) guide.
Promoting Interoperability includes an automatic exception for small practices (15 providers or less). The 25% will automatically be allocated towards the Quality and Improvement Activities measures.
A practice’s performance across the 4 MIPS categories (or less if reweighted) will result in a MIPS final score of 0 to 100 points.
A practice’s MIPS final score will determine whether they receive a negative, neutral, or positive MIPS payment adjustment.
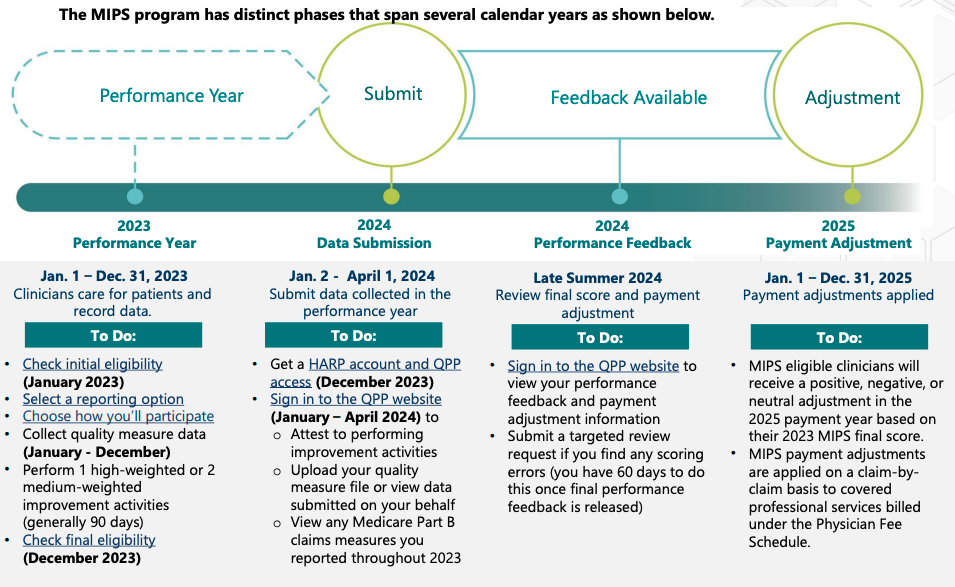
Performance in 2023 will determine adjustments to payments in 2025, equaling +/- 9% of practices’ 2025 payments (applicable only to Medicare Part B Physician Fee Schedule payments).
To receive a neutral adjustment (i.e. avoid penalty), practices must earn at least 75 total points if they are required to participate.
After determining your MIPS eligibility and participation level, your practice can begin selecting and performing your measures and activities. To start, here is a timeline for each category:
| Quality | Cost | Improvement Activities | Promoting Interoperability |
|---|
| Clinicians must select 6 measures, collecting data for each measure for the 12-month performance period (Jan 1 - Dec 31, 2023) | No action needed to collect or submit any data for cost measures. CMS calculates your Cost performance through your claims. | Clinicians must select between 2 and 4 activities, performing each activity for a continuous 90-day period in Calendar Year (CY) 2023 | Most clinicians must collect data using CEHRT on the required measures for the same continuous 90- day performance period in CY2023.
Small practices (practices with 15 or fewer providers) are automatically excused from the PI category. |
If your practice is participating in MIPS 2023, you will submit data following the performance year between January 2 - April 2, 2024 . See the timeline below for steps once the performance year finishes:
The QPP has released a helpful Small Practice Action Planning Tool. If you are in a small practice, or plan on reporting traditional MIPS, this guide provides a step by step tool kit to understand areas for improvement on previous MIPS scores to focus on in 2023.
*This article is provided for instructional purposes only. Elation Health does not support or guarantee anything other than relay useful information from various organizations. Elation Health also does not provide support for third-party technologies. We recommend consulting CMS guidelines for the most up to date information.
Copyright U.S Centers for Medicare & Medicaid Services. All rights reserved.
Related Articles



