Table of Contents
Every
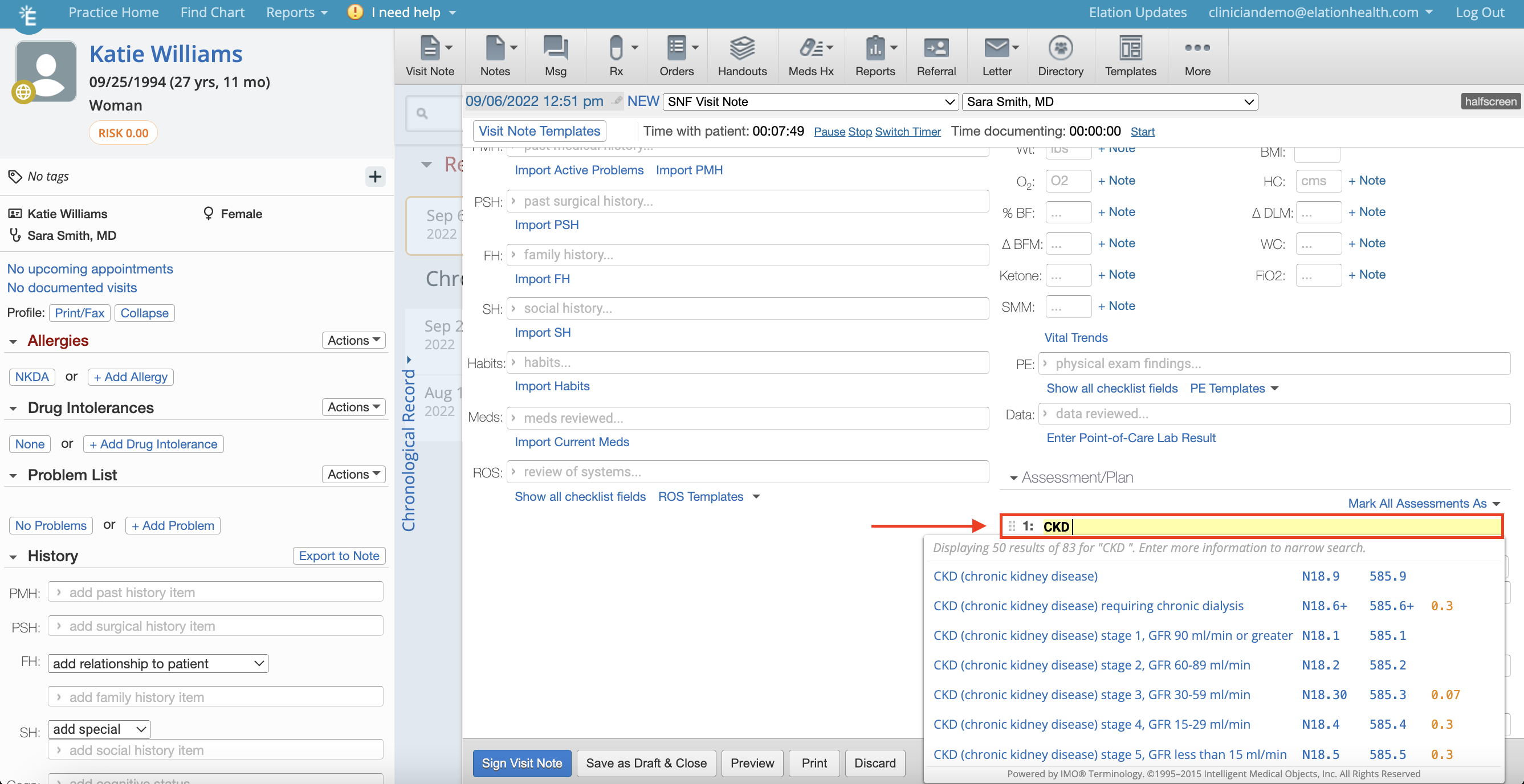
Visit Note Format in Elation contains an
Assessment field except for the Simple Note. There are two ways to document clinical assessments during a patient encounter.
- You can type out a text narrative in any of the assessments fields in Elation
- You can use the ICD database to enter coded assessments in any of the H&P and Pre-Op Visit Note formats.
Write out a narrative assessment in any of the assessment text fields in any of the visit note formats available. If a drop down appears with diagnosis codes you can bypass the drop down and keep typing if desired. The text box will continue to expand to allow you to type as much text as needed. If you choose to use
coded assessments, see below.
By default, the
Coded Visit Note Assessments feature is turned on for providers in the
Preferences section of their Elation Settings upon account creation. The following workflow applies to any of the
H&P and
Pre-Op Visit Note formats only.
- Click into the Assessment field
- The patient's list of active problems from their Problem List will appear immediately below. Click a problem from the list to apply it as an assessment, or start typing to find a different assessment from the ICD database.
- When you start typing, Elation will return search results from our ICD database.
- Select the appropriate diagnosis from the list to apply it as an assessment. It will be added to your visit note along with its corresponding ICD-10 code(s).
- The ICD-10 code associated with the diagnosis selected will also be automatically added to the billing section of your visit note.
- After you select a diagnosis from the search results, you can also edit its description by changing the text that is pre-filled in the assessment field:
The patient's list of active problems from their Problem List will appear immediately when you click into the Assessment field in any of the H&P and Pre-Op Visit Note formats to allow you to use data already stored in the Problem List in your visit note documentation.
You can also add a new assessment from your visit note documentation back to the Problem List directly from your visit note to make it easy for you to keep all problems in one place. Follow the steps below to accomplish this.
- If you document a new chronic issue for the patient that you want to add to the patient's Problem List, click the "Add Problem" button that appears to quickly add it to the patient's Problem List.
- The problem will immediately show up at the bottom of the patient's Problem List with the description that you entered in the Assessment field, ICD-10 code and today's date. Click "Actions" >> "Edit" to edit the details of this problem as needed.
By default, ICD-10 codes for your Assessments will show up in your visit note when you print, fax, or share them.
If you do not want Dx codes to show up alongside the assessments in your visit note
, you can turn this off in "Settings" >> "Preferences", under
Coded Visit Note Assessments. The toggle will be set to "Yes" by default. Change it to "No" to remove Dx codes from your visit note documentation.
Next Step
Utilize the coded assessments feature today to assist with billing and keep your Problem List up to date!
Related Articles



