Contents
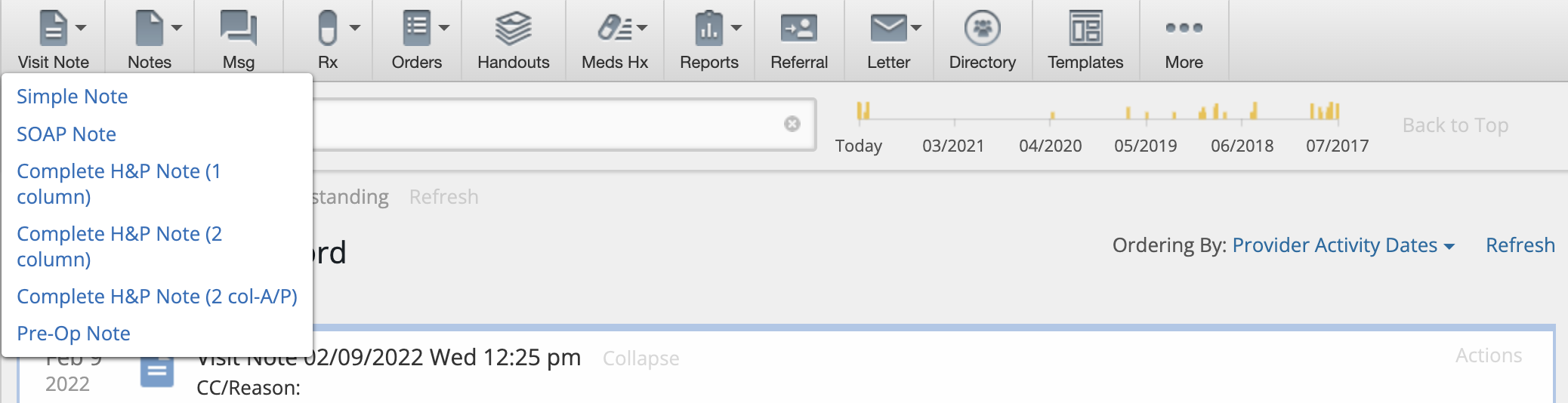
In Elation, there are 6 different Visit Note Formats that provide you with different layouts for storing clinical information when documenting a clinical encounter. Each layout has its own characteristics that makes it suitable for different documentation workflows and preferences. You can find the different visit note formats under the "Visit Note" button in the gray navigation bar.
Every Visit Note Format has the following default sections and fields:
The Simple Note contains a single blank text box that is ideal for customers who are free-texting a long narrative or for use with dictation softwares or external templating softwares. You can also
- click "+ Add Vitals" to separately record patient vitals
- click "+ Add procedure" button to separately record detailed procedure information
- click "+ Add instr" to separately note instructions to patients
The SOAP Note is broken down into 4 text boxes, Subjective (Prob), Objective, Assessment & Plan. This allows you add more granularity to your narrative than a
Simple Note would while still allowing you to easily utilize dictation softwares or external templating softwares. You can also:
- click "Import Current Meds" to easily reference patient medication information into the Problem box
- click "+ ros" to separately record Review of Systems information
- click "+ Add Vitals" to separately record patient vitals
- click "+ pe" to separately record Physical Exam information
- click "+ Add procedure" button to separately record detailed procedure information
- click "+ Add instr" to separately note instructions to patients
The Complete H&P Note (1 column) allows you to store detailed history and physical examination information in a single column format and allows you to import data directly from the Clinical Profile into your visit note with the various "Import" buttons in each section of the note. You can also:
The Complete H&P Note (2 column) uses the traditional SOAP methodology but offers more structure for viewing everything on a single screen by placing the Subjective data on one side and Objective, Assessment and Plan on the other.
You can click the "Import..." buttons to import information from the Clinical Profile into the visit note and you can also export data from your visit note back to the Clinical Profile. This way you never have to double document! Click the "add..." button that appears next to the new data you enter into any of the fields available in the Clinical Profile to add the new data to your Clinical Profile.
The Complete H&P Note (2 col-A/P) is the same as the
Complete H&P Note (2 column) except the Assessment and Plan sections are combined.
The Pre-Op Note is the same as the
Complete H&P Note (1 column) with the addition of the
Date,
Consultant and
Attending fields to note additional details about the operation or procedure that the patient is scheduled for.
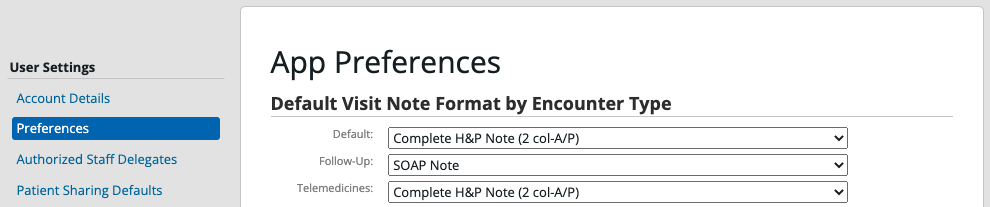
Each provider can set their default Visit Note format by going to "Settings" >> "Preferences" >> "App Preferences". They can also associate default Visit Note formats by their Encounter Types (Appointment Types) in the same page or in the Calendar & Booking Settings page under each Appointment.
Next Step
Review the different visit note formats and choose your default!
Related Articles



